Explore symptoms, diagnosis, treatments, and the latest research on Inflammatory Bowel Disease (IBD).
Guest post by Hema Cherukooru
Inflammatory bowel disease (IBD) is characterized by repetitive inflammation of the gastrointestinal tract. Crohn’s disease and ulcerative colitis are chronic IBD conditions that are emerging as worldwide epidemics. They occur after an abnormal immune response to normal stimuli such as food and an inappropriate immune response to intestinal flora in genetically susceptible individuals. IBD usually occurs in people aged 15 to 30 years old, and seems to be more prevalent in Europe and North America than in Africa or Asia.[1,2]

The intestine acts as a barrier and prevents bacteria and antigen from entering the circulation. However, in the case of IBD the barrier function of the intestine is defective and leads to inflammation. Crohn’s disease and ulcerative colitis differ in their clinical and pathophysiology, but are defined as chronic IBD. Crohn’s disease can affect any part of the GI from mouth to anus and appears as patches of healthy tissue next to damaged parts. The mucosa has a cobblestone like appearance. Ulcerative colitis affects the large intestine and rectum and the damaged areas are continuous.[3]
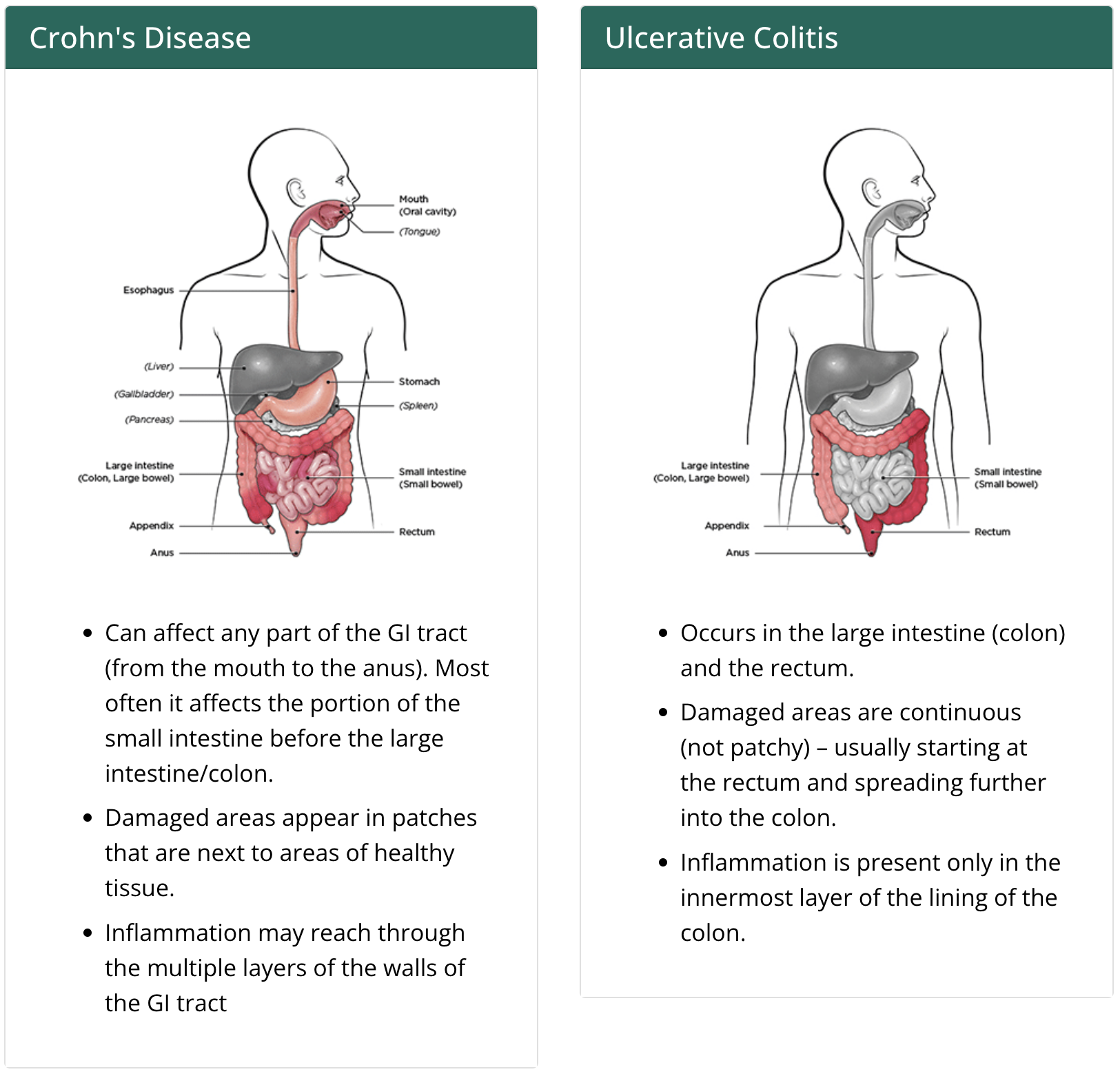
Image credit: CDC.gov
Risk factors for developing IBD include:
- Age: Most common in ages 15 to 30 years old. In some cases, it can develop in 50 and 60-year-olds.
- Family history: Increased risk when close family members are affected.
- Race and Ethnicity: Can occur in all races but whites are most susceptible.
- Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs increase the risk of developing IBD or worsen IBD.
- Cigarette smoking: Most controllable factor to prevent Crohn’s disease. In case of ulcerative colitis, smoking may help prevent it, but the benefits of quitting smoking helps overall health and outweighs this benefit.
Common symptoms include:
- Fatigue,
- Persistent diarrhea,
- Rectal bleeding/bloody stools,
- Abdominal pain, and
- Weight loss.
Diagnosis:
Healthcare professional would look for a combination of the following to help with diagnosis IBD: Clinical findings, Inflammation lab markers, Image findings, and Endoscopy or colonoscopy helps confirm IBD.
Treatment:
Treatment depends on the management of mild, moderate, and severe disease. Goal is to induce remission of Crohn’s disease or ulcerative colitis. The treatment options vary depending on the patient’s condition from medication like glucocorticosteroids, immunomodulators, and/or antibiotics, and surgery may be required.
Key micronutrients patients are risk of developing deficiency of the following (Please note this is general information and each individual should consult their healthcare professional): Iron deficiency or anemia, Vitamin D, Calcium, Zinc and Magnesium in case of chronic diarrhea.
Complications of IBD may include:
Increased risk of blood clots. Medication side effects, for example corticosteroid can lead to high blood pressure and osteoporosis. Increased risk of colon cancer. Inflammation may occur during IBD flare ups.
Dietary guidelines:
No evidence that what you eat can cause IBD, however, certain foods can trigger signs and symptoms. Some of the general guidelines to manage symptoms include:[4,5,6,7]
- Limit dairy products, many people with IBD have symptoms such as diarrhea, gas, abdominal pain and limiting or eliminating dairy would be helpful.
- Drinking plenty of liquids daily, especially water would be helpful. Avoid alcohol and caffeinated beverages as they make diarrhea worse by stimulating the intestine. Carbonated drinks produce gas and should be avoided as well.
- Small meals about five to six a day would be better than two to three large meals.
- Low FODMAPs (Fermentable oligosaccharides, disaccharides, monosaccharides and polyols) diet.
- Omega-3 fatty acids supplementation.
- In case of vitamin or mineral deficiency, supplements taken as needed.
- Modify fiber intake, in case of high risk of obstruction, a low-fiber diet may be recommended. In Crohn’s disease a low-residue diet, did not change the outcome.
- If uncontrolled weight loss occurs or if the diet is very limited, consult a registered dietitian.
- In case oral feeding is not sufficient, patient may be started on enteral or parenteral feeding.
Stress
Stress and its relation to Crohn’s disease is controversial. However, patients have reported during high stress periods, symptoms flare. Managing stress by the following strategies might be helpful :
- Exercise – Mild exercise can help relieve depression, reduce stress, and normalize bowel movement. Doctor should be consulted for an exercise plan.
- Breathing exercise and regular relaxation – Yoga, mediation, and practicing deep and slow breathing might be helpful.
Coping and Support for patients with IBD
IBD affects patients physically and emotionally, as it could disrupt daily life due to flaring of symptoms and the need to use restroom more often. Some of coping strategies could include:[6]
- Be informed of IBD and seek information from respectable sources such as Crohn’s and Colitis Foundation.
- Joining support groups helps on the emotional level as well as to get updates on the latest medical treatments therapies available.
- Consult a mental health professional who specializes in IBD if needed.
Once an individual is diagnosed with IBD, it would be helpful to learn how to manage symptoms and prevent flare-ups and worsening of the condition. Role of health care professional to key to managing IBD. In case of uncontrolled weight loss, a registered dietitian may need to be consulted. (Click here to schedule a virtual call with Dina and here to learn more about our self-paced online courses for IBD and other conditions.)
Please join us in acknowledging IBD during World IBD Day in May and Crohn’s and Colitis Awareness Week in December.
Hema Cherukooru is a dietetics student at the University of Northern Colorado pursuing a Bachelor’s Degree in Nutrition and Dietetics.
References:
- McDowell, C., Farooq, U., & Haseeb, M. (2020). Inflammatory Bowel Disease. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK470312/
- Manichanh, C., Borruel, N., Casellas, F., & Guarner, F. (2012). The gut microbiota in IBD. Natural Review. Gastroenterology & Hepatology, 9(10), 599-608. doi: 10.1038/nrgastro.2012.152.
- CDC.Inflammatory bowel disease (IBD) (2018). What is inflammatory bowel disease (IBD)? Retrieved March 3, 2021, from https://www.cdc.gov/ibd/what-is-IBD.htm
- Mayo Clinic (n.d.). Inflammatory bowel disease (IBD). Retrieved March 3, 2021 from https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/symptoms-causes/syc-20353315
- Halmos, E.P., & Gibson, P.R. (2015). Dietary management of IBD — insights and advice. Nature Reviews. Gastroenterology & Hepatology, 12(3), 133146. https://doi.org/10.1038/nrgastro.2015.11
- Mayo Clinic (n.d.). Inflammatory bowel disease (IBD). Retrieved March 15, 2021, from https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/diagnosis-treatment/drc-20353320
- Gibson, P. R. (2017) The evidence base for efficacy of the low FODMAP diet in irritable bowel syndrome: is it ready for prime time as a first-line therapy?. Journal of Gastroenterology and Hepatology, 32: 32–35. doi: 10.1111/jgh.13693.



0 Comments