Learn about the types of diabetes, prevention strategies, and lifestyle tips to manage this condition effectively. Discover how nutrition plays a crucial role in diabetes prevention and care.
My very first job as a Registered Dietitian (RD) was in a high-risk obstetrician-gynecologist (OB-GYN) office in midtown Manhattan. The majority of my patients were pregnant people diagnosed with gestational diabetes, something I only learned about in my school textbooks but had no real world experience with at the time. Lack of knowledge didn’t stop me from diving in and consulting every resource possible—human and otherwise—so that I could be of service to this population.
During my four years in that office, I was also trained—twice—by the Centers for Disease Control and Prevention (CDC) as part of its “Prevent Type 2” National Diabetes Prevention Program. Every week for an entire year, I would meet with dozens of people from our local community at our neighborhood community center and review the CDC’s curriculum and lessons on helping folks decrease their risk of getting diabetes.
Suffice it to say that, over my 8-year stint so far as an RD, I’ve probably worked with thousands of people who are managing some form of diabetes or have been told they’re at risk for diabetes. Am I an expert in this condition? Probably not as there are so many complex, challenging, and individual factors to consider. Granted, anyone can look online to find recommendations and guidance about managing diabetes, but being an RD means that I have to customize my approach to determine the best treatment for each person.
With over 38 million Americans, currently diagnosed with diabetes, and a global projection of about 783 million by 2045, it makes sense to have public health efforts in place to prevent and manage this chronic condition.
Diabetes Awareness Month, observed every November, is a campaign to raise awareness about diabetes and its impact worldwide. The initiative highlights the importance of education, prevention, and effective management of diabetes, aiming to support the millions affected by this chronic condition. Key efforts include community engagement activities, such as advocacy, fundraising, and educational events, which foster understanding and empower those living with diabetes.
Similarly, World Diabetes Day, celebrated annually on November 14, is the largest global awareness campaign for diabetes, uniting over a billion people across 160 countries. Each year, the campaign spotlights the increasing impact of diabetes on individual and public health, focusing on a key theme to drive advocacy and education efforts. From 2024 to 2026, the theme “Diabetes and Well-being” highlights the importance of holistic approaches to diabetes management, emphasizing mental and emotional support alongside medical care. This global initiative encourages individuals, communities, and governments to engage in prevention, improve access to quality care, and advocate for policies that support those affected by diabetes.
What Is Diabetes?
Not all diabetes diagnoses are created equally; in fact, the term “diabetes” encompasses multiple types with distinct causes, characteristics, and treatment approaches. The most common forms are listed below. Other less common forms of diabetes, such as monogenic diabetes, also highlight the diversity within diabetes diagnoses, underscoring the need for tailored treatment and management strategies for each individual case.
Generally speaking, diabetes is a chronic condition where a person’s blood glucose (blood sugar) levels are consistently elevated. Glucose (the sugar molecule found in carbohydrate foods) is crucial for energy in the body, and insulin, a hormone produced by the pancreas, helps regulate its absorption into cells. Poorly controlled diabetes can lead to complications across nearly all systems of the body—heart, eyes, kidneys, skin—as well as amputations, or even death.
How Diabetes Is Diagnosed
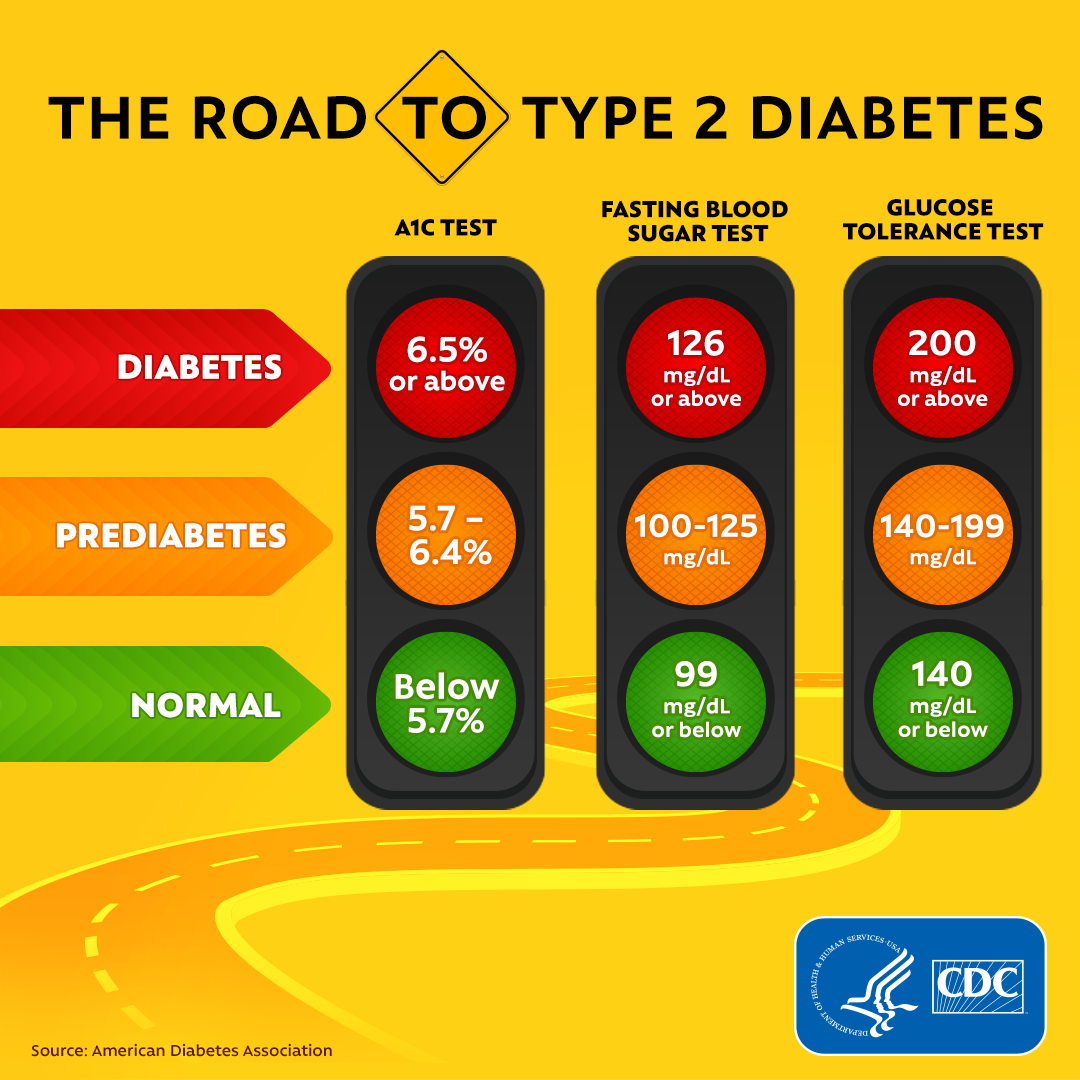
To diagnose diabetes, healthcare providers typically use the following tests:
- Fasting Plasma Glucose (FPG) Test: Measures blood glucose after fasting overnight.
- A1C Test: Shows average blood sugar levels over the past 2-3 months.
- Oral Glucose Tolerance Test (OGTT): Involves fasting, then drinking a sugary solution, and testing blood sugar levels after 2 hours.
These tests help diagnose diabetes, prediabetes, and gestational diabetes by assessing blood glucose levels under different conditions. If results indicate diabetes, further testing and evaluation are usually recommended to confirm the diagnosis and determine appropriate management.
Preventive Interventions and Lifestyle Modifications
Because blood glucose levels are so closely tied to carbohydrate intake, your healthcare provider might prescribe insulin or another form of medicine and ask you to use finger sticks and a glucose meter to log your numbers over the course of a day. In some cases, this is going to be critical to keep control; in other cases, there may be more flexibility.
Type 1 Diabetes is an autoimmune condition, typically diagnosed in childhood (which is why it was formerly called juvenile diabetes), in which the body does not produce enough insulin to stabilize blood glucose levels. There’s no way to prevent Type 1 diabetes because there doesn’t seem to be a specific trigger for it, though some factors may play a role, such as genetics, viruses, dietary factors, or toxins. Insulin management is absolutely essential to support the body’s inability to produce insulin.
- INSIDE SCOOP: Check out our podcast episode with Jessica Freeman for her personal insight as a person living with Type 1 Diabetes:

Prediabetes is often diagnosed by a blood test that determines if someone is on the border (see the chart below). The emphasis to reverse this condition and stave off progression to Type 2 is usually focused on creating a balanced diet, including regular physical activity, weight management, and stress reduction.
Type 2 Diabetes is the most common form of diabetes and primarily develops due to insulin resistance, where cells in muscles, fat, and the liver do not respond effectively to the insulin being distributed in the body. Risk factors may include excess body fat, physical inactivity, genetics, and family history. Education and counseling around nutritional guidelines is usually the first form of treatment for maintaining stable blood sugar levels and may include practical tips on meal planning, mindful eating, and nutrient timing.
- SIDE NOTE: While I love the diversity of this meal plan—and the fact that it was created by a dietitian colleague—I find it falls short of the average daily caloric intake for an adult. I’d recommend doubling up on some of the protein-rich foods or supplementing with a heartier side dish for satiety.
Gestational diabetes occurs during pregnancy and can create potential risks for both the pregnant person and the child. The mere fact that one is pregnant can be risk factor enough (aka, the “diabetogenic state”) if the body cannot produce enough insulin during pregnancy to meet its increased needs, leading to high blood sugar levels. Managing gestational diabetes typically involves diet, exercise (with medical clearance), and sometimes blood sugar monitor as fluctuating hormones can make this condition more challenging.
Type 3 Diabetes is a developing term often linked to cognitive decline and Alzheimer’s. The overview of current research seems to be based more in theories than hard evidence, but I think we may start seeing some updates about this soon.
JOIN US!
If you’re reading this before November 14, click here to join our FREE webinar to learn all about preventing and managing Type 2 Diabetes. As always, registrants will receive a link to the recording after the event, so don’t worry if you can’t attend the live event. Or you can head to our Wellness Webinar playlist on DishWithDinaTV to check out past events on similar topics.
References
- Diabetes Awareness Month
- World Diabetes Day
- What Is Diabetes?
- Catalano, P., (2002). The Diabetogenic State of Maternal Metabolism in Pregnancy. Neoreviews, 3 (9): e165–e172. https://doi.org/10.1542/neo.3-9-e165
- Vounzoulaki, E. (2020). Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ 2020; 369 doi: https://doi.org/10.1136/bmj.m1361
- de la Monte, S. M., & Wands, J. R. (2008). Alzheimer’s disease is type 3 diabetes-evidence reviewed. Journal of diabetes science and technology, 2(6), 1101–1113. https://doi.org/10.1177/193229680800200619
- Understanding Diabetes Diagnosis


0 Comments