Discover the differences between food allergies and intolerances, learn about common symptoms, and gain insight into making safe food choices.
Food allergies and intolerances affect millions worldwide. Understanding the difference is crucial, but can also be complex, challenging, and confusing for those managing their conditions.
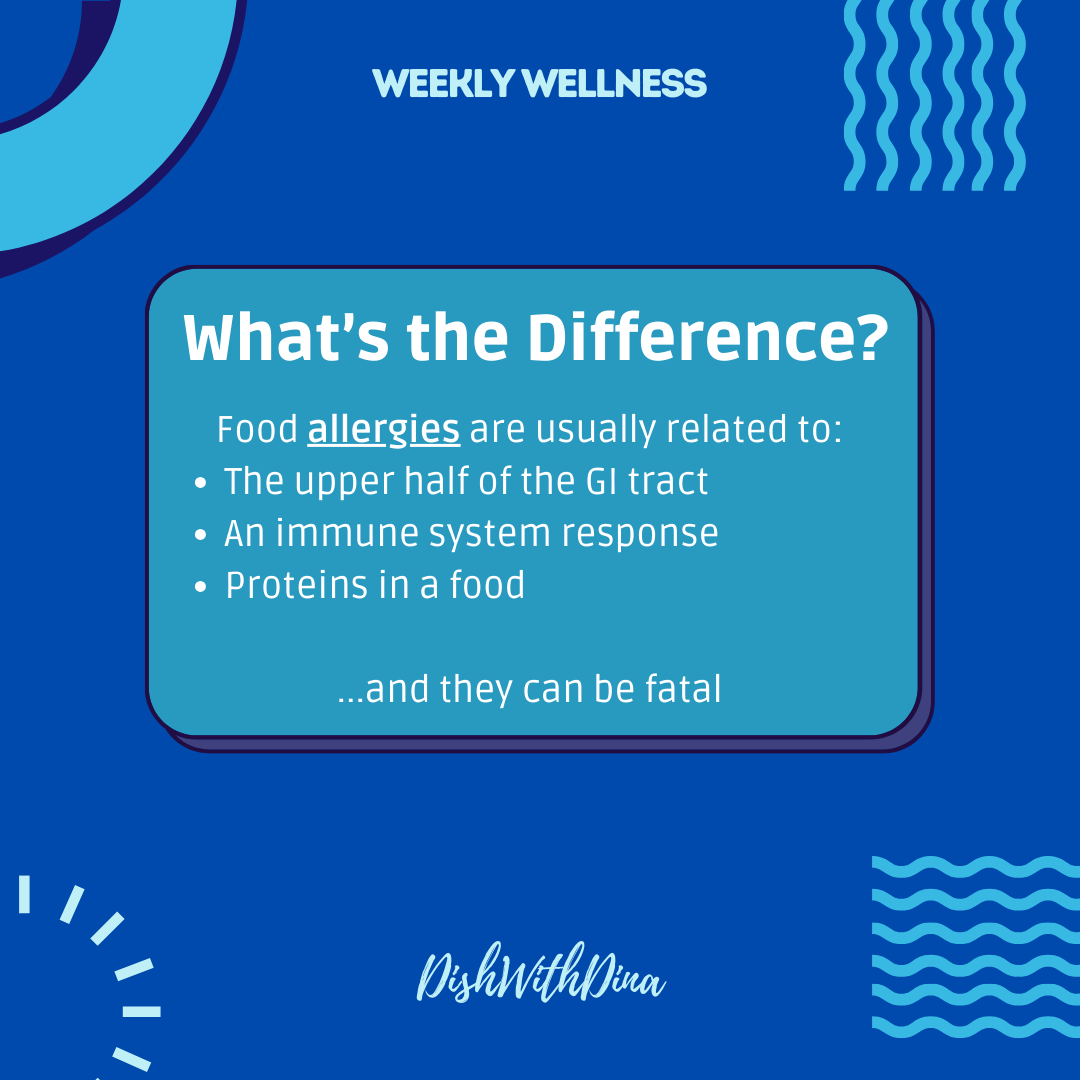
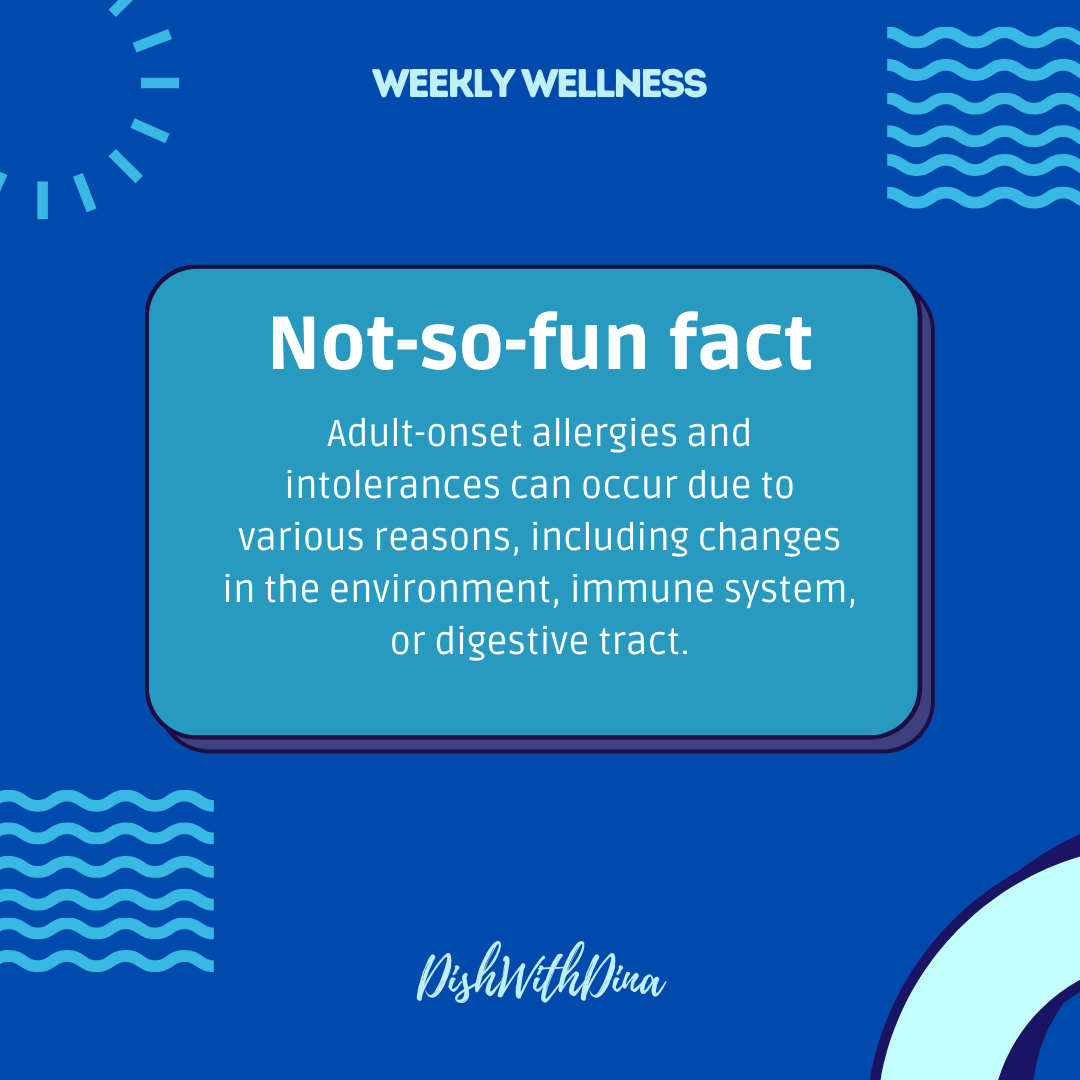
Food allergies are an immune system response that is triggered by specific proteins in certain foods [1]. These allergies can result in a range of symptoms, from mild reactions like hives to severe and life-threatening anaphylaxis. The top 9 food allergens in the United States are: peanuts, tree nuts, sesame, milk, eggs, soy, wheat, fish and shellfish [2]. It’s vital for those with allergies to read food labels carefully, avoid allergens, and prevent cross-contamination when preparing meals at home or dining out. While it is possible that some may outgrow their allergies (just as adult-onset allergies are possible), others, particularly peanut allergies, may persist throughout life.
Immunocompromised Populations
Individuals undergoing chemotherapy, organ transplant recipients, seniors, infants, or those living with HIV/AIDS are particularly vulnerable to complications around food allergies and intolerances. Their weakened immune systems make them more susceptible to severe allergic reactions and complications from consuming allergenic foods. Therefore, it’s crucial to exercise extreme caution when dealing with food allergies, especially regarding cross-contamination.
Cross-contamination can occur easily in both home and restaurant settings, posing a significant risk to immunocompromised individuals [3]. Simple preventive measures, such as thoroughly washing utensils, countertops, and cutting boards after each use, are essential. If you have a food allergy, be sure to communicate your dietary needs when dining out or heading to an event or outside venue. Ask about food preparation methods to avoid accidental exposure to allergens. By being vigilant and proactive, immunocompromised individuals can better safeguard themselves against the risks associated with food allergies and intolerances.
Food Intolerances
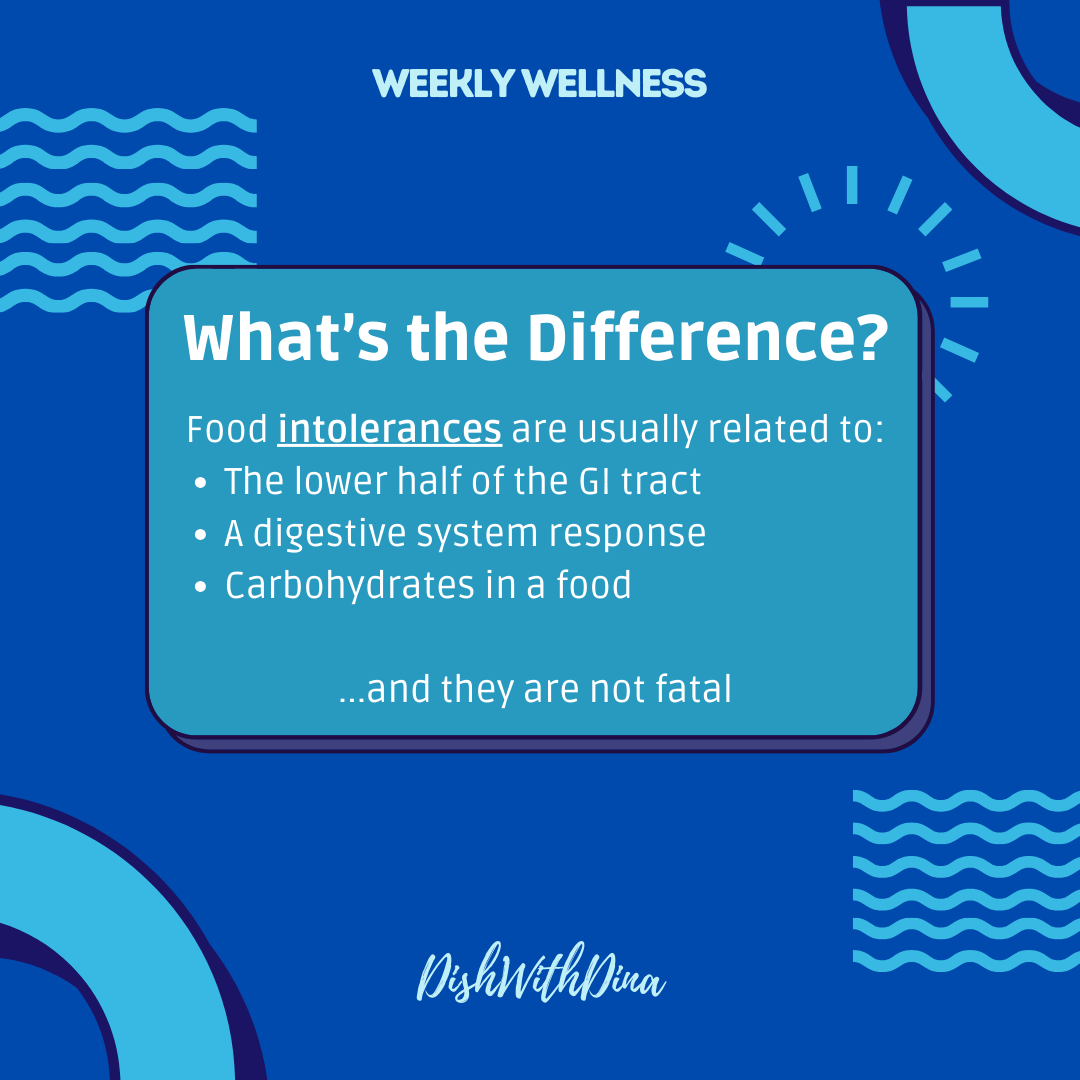
Food intolerances are less severe than allergies, but can be as challenging to live with. These involve the digestive system’s sensitivity to certain carbohydrates; therefore, symptoms are usually lower in the gut, such as bloating, cramping, and diarrhea. For individuals seeking to identify their food triggers, a short-term elimination-reintroduction diet under a Registered Dietitian’s supervision may be beneficial [4]. Some of the top intolerances are listed below:
- Lactose, a naturally occurring sugar found in milk
- Gluten, a protein found in certain grains like wheat, barley, rice
- Caffeine, the stimulant found in coffee and some teas
- Salicylate, a chemical compound in aspirin, but also in legumes (e.g., lentils, beans), vegetables (e.g., cauliflowers, pickled vegetables), fruits (e.g., strawberries, plums, watermelons, raspberries), and some cereals (e.g., buckwheat, oat or corn), herbs and spices
- Amines, chemical compounds found in some aged, pickled, smoked, canned or dried food products
- FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), the group of short-chain carbohydrates that are sometimes poorly absorbed in the small intestine
- Sulfites, used as preservative in food items such as beer, wine, lemon juice, molasses, sauerkraut, gravies, soft drinks, fruit juices; shrimp, lobster and other crustaceans; dough foods like biscuits, pie and pizza crusts.
- Artificial sweeteners, sugar substitutes (often used by people with diabetes to help control their blood glucose) that taste sweet but don’t contain table sugar; brand names include Nutrasweet®, Equal®, Sweet and Low®, and Splenda®
Getting Diagnosed
There are several methods to diagnose a food allergy, some of which may be used in combination [5]. Working with a qualified healthcare professional can help accurately identify food allergies and develop appropriate management strategies.
- Skin Test: A skin prick test involves pricking the skin with a tiny amount of the suspected allergen and observing for a reaction, such as redness or swelling.
- Blood Test: A blood test, also known as specific IgE testing, measures the levels of allergy-causing antibodies in the blood in response to specific foods.
- Oral Food Challenge: In this controlled setting, the patient consumes small amounts of the suspected allergen under medical supervision to observe for allergic reactions.
- Elimination Diet: This involves removing suspected allergens from the diet and then gradually reintroducing them to identify the culprit.
- Medical History and Physical Examination: A thorough assessment of symptoms, medical history, and physical examination can provide valuable clues to guide further diagnostic testing.
Food intolerances are diagnosed through different methods to determine patterns of trigger foods and symptoms, including:
- Elimination Diet: This involves systematically removing suspected foods from the diet and monitoring for symptom improvement. Foods are then reintroduced one at a time to identify which ones trigger symptoms.
- Food Diary: Keeping a detailed food diary can help track symptoms and identify patterns of food intolerance.
- Special Diets: Under medical supervision, individuals may follow specialized diets to pinpoint specific intolerances.
- Medical Assessment: Healthcare professionals may conduct physical examinations and evaluate medical history to rule out other conditions and narrow down potential causes.
- Food Intolerance Tests: While available, the accuracy and effectiveness of these tests can vary, and they are often considered controversial. They may include blood tests or other diagnostic methods to measure the body’s response to certain foods [6].
Managing Your Condition
Living with food allergies or intolerances can be challenging, but you can still enjoy delicious meals with the right approach. Here’s how:
- Stay Regular: Check-ups and discussions with your healthcare professionals—including a Registered Dietitian—can help you manage and monitor your condition effectively.
- Read Labels: Always check food labels for allergen information or trigger ingredients. (Food manufacturers are required to list common allergens on packaging.)
- Cook at Home: Preparing meals at home can give you full control over ingredients and cross-contamination.
- Plan Ahead: When dining out, call ahead to discuss your dietary needs with the restaurant staff. Restaurants and foodservice establishments are increasingly mindful of food allergies and may offer allergen-free options. In fact, some resources have already taken the guesswork out for you. For instance, if you’re in New York City, check out Allergy Eats.
- Support Groups: Connect with local or online support groups for advice, recipes, and emotional support from those who understand your challenges.
- Stay Positive: Remember that many delicious foods are naturally allergy/intolerance-friendly. Explore new recipes and ingredients to keep your meals exciting!
Being a Registered Dietitian qualifies me to work with various ages, populations, and conditions, but food allergies and intolerances are always a bit tricky as I find that I need to take the most individualized approach when patients show up with these conditions. To provide some insight into my approach, I usually focus on the following:
- Patient Education: I never assume a patient understands their condition or how to manage it. It’s a sad and frustrating fact that some people who work with me get their diagnosis, receive a handout, and are sent on their way. I prioritize educating patients about their specific food allergies or intolerances. This includes explaining the difference between the two, common symptoms, and potential dietary modifications.
- Nutritional Guidance: I provide personalized nutritional guidance tailored to each patient’s needs and preferences. This may involve reviewing meal plans that exclude allergens or trigger foods while ensuring balanced nutrition.
- Navigating Challenges: So many challenges can be related to food allergies and intolerances, especially when dining out, attending social gatherings, and traveling. Some of the strategies my patients and I work on include reading food labels, communicating with restaurant staff, and planning ahead.
- Support and Empowerment: Unfortunately, food allergies and intolerances can lead to fear and disordered eating. Some patients may become overly vigilant about their food choices which result in restrictive eating patterns and fear of consuming certain foods, potentially leading to micronutrient deficiencies [7]. Additionally, not only can the physical symptoms be challenging to manage and contribute to disordered eating behaviors, but so can the psychological impact of food allergies, including anxiety and stress,

Play It Safe
If you’re reading this before May 16, 2024, click this link to register for our *FREE* monthly wellness webinar where we’ll be diving deeper into the details around food allergies and intolerances. Can’t make the live event? No sweat! All registrants will receive a link to the recording after the event. Missed the registration? Not a problem! Head to our podcast or YouTube channel to catch the replay.
Consider including these versatile and allergen-free recipes into your next week’s meal plan:
- Quinoa Salad – can be customized with various veggies and dressings
- Lentil Soup – hearty option packed with nutrients and flavor
- Banana Bread – a gluten-free treat
- Energy Bites – an allergy-friendly snack made with seeds, dried fruits, and oats
References
- https://www.foodallergy.org/
- https://www.fda.gov/food/food-labeling-nutrition/food-allergies
- https://www.fsis.usda.gov/news-events/events-meetings/food-safety-education-month-preventing-cross-contamination
- https://www.foodallergy.org/our-initiatives/awareness-campaigns/food-allergy-awareness-week
- https://www.niaid.nih.gov/diseases-conditions/diagnosing-food-allergy
- https://my.clevelandclinic.org/health/diseases/21688-food-intolerance#diagnosis-and-tests
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10765559/



0 Comments